- A-
- A+

CATARACT SURGERY
Cataract surgery is a routine, effective procedure for restoring eyesight: find out about cataract symptoms, progression and recovery after surgery.
Cataract is a common eye disease and the leading cause of visual impairment across the world (48% of cases). The only option is surgical treatment.
WHAT IS cataract?
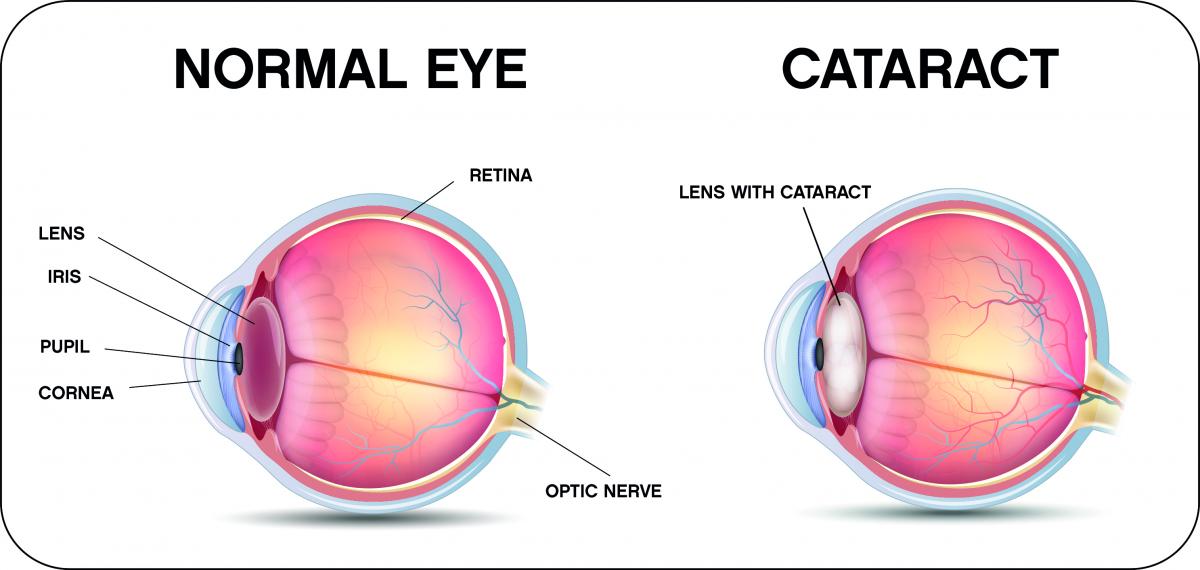
A cataract is clouding of the lens. The lens is a natural structure located inside the eye behind the iris (the coloured part of the eye). The lens is crucial for sight and also for visual accommodation, i.e. the ability to switch between near and far focus.
The commonest cause of cataracts is age and therefore ageing, but cataracts can also result from eye injury (post-traumatic cataract), a pre-existing eye disorder (pigmentary retinopathy, previous eye surgery, etc.), medical treatment (corticoids, orbital radiotherapy, etc.), or chronic illnesses such as diabetes. In children, cataract can also be congenital.
A number of factors increase the risk of developing cataracts, including smoking, excessive alcohol consumption and exposure to sunlight (ultraviolet rays).
cataract SYMPTOMS
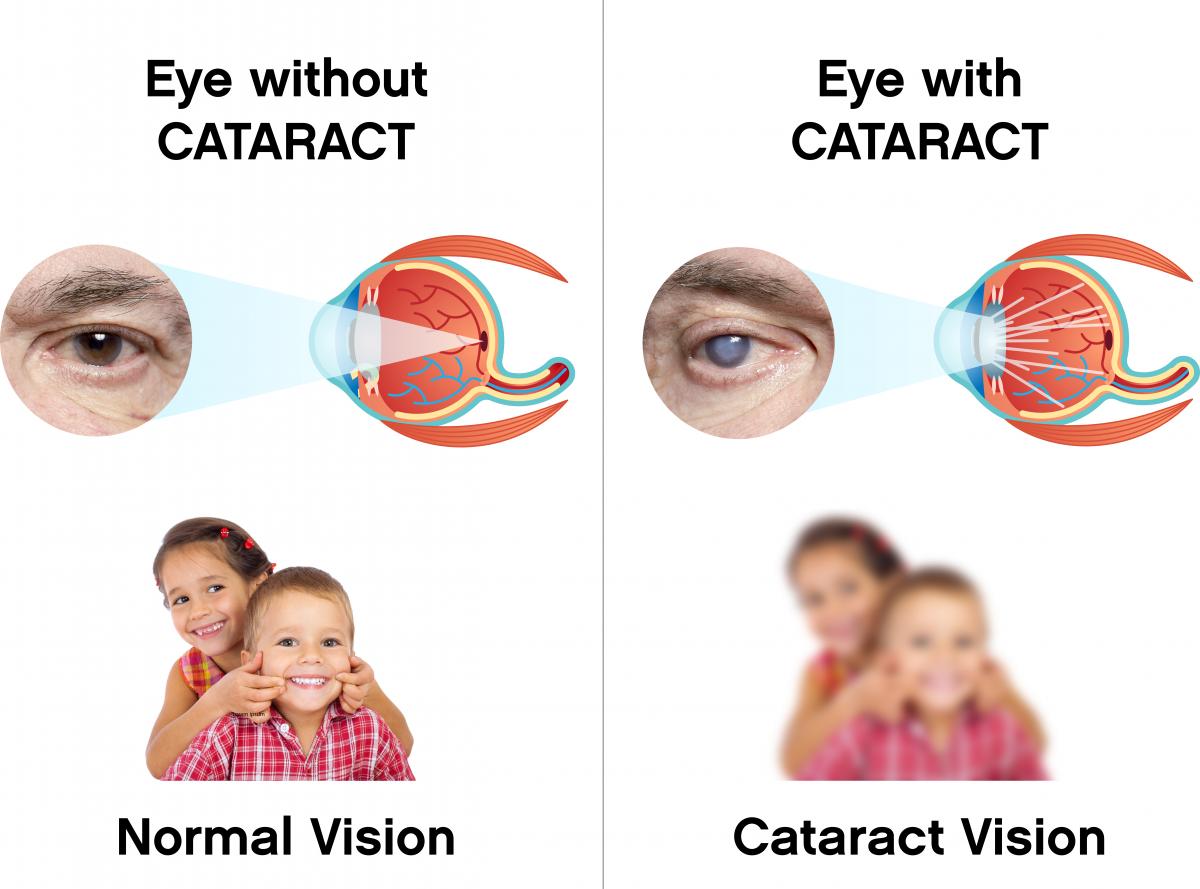
As we get older, the normally transparent crystalline lens becomes increasingly opaque. Light has difficulty passing through this lens and reaching the retina. This prevents images and colours from being correctly perceived.
Cataract do not develop evenly and at the same rate. They can form in one eye only, or more commonly in both, leading to blurred or misty vision and progressive impairment of eyesight that cannot be corrected by wearing glasses.
Other symptoms may also appear:
- small blotches or tiny specks in the field of vision
- problems perceiving contrast, relief or colours
- seeing things as if through a veil
- difficulty reading and increased sensitivity to light, including glare, particularly when driving at night
- double vision in one eye
A cataract can also have an effect on the strength of your glasses, leading to short-sightedness or making existing short-sightedness worse and therefore impairing long distance vision.
An ophthalmic exam, is crucial for reaching a diagnosis. Patients must be assisted by their ophthalmologist, who will inform them when the time has come for surgery based on the degree of visual impairment.
ophtalmologIC TREATMENT FOR cataractS
There is no existing medical treatment for cataracts; the only treatment option is surgery. It is a well-established technique and, in the majority of cases, has highly satisfactory results.
However, if there are no symptom or vision is only slightly affected, a cataract operation may not be necessary. In such cases, it may be sufficient simply to change the prescription of your glasses. Your ophthalmologist will assess whether surgery is necessary based on the impact of impaired vision on your everyday activities (reading, driving, leisure pursuits, etc.).
If no surgery is performed, the lens will become increasingly cloudy. This will affect your eyesight and ultimately your independence. This is why you should have regular eye tests so that your ophthalmologist can assess the situation.
The main contraindications for cataract surgery are: the patient finds that simply wearing glasses solves the problem, the patient has an associated condition that would make surgery risky, or that proper post-operative care and follow-up cannot be ensured.
SURGICAL TREATMENT FOR cataract
Cataract surgery involves removing the lens and replacing it with a synthetic one, called an “intra-ocular lens implant” or “artificial lens”.
Some implants can also help correct presbyopia, short-sightedness and astigmatism (malformed cornea), thus making it unnecessary to wear glasses for short-sightedness or long-sightedness.
Stages of cataract surgery
Hospitalisation is not necessary; the operation is usually performed in the Outpatient Department. The operation itself takes around fifteen minutes. It is performed in a sterile operating environment. Surgery is done with the patient lying on their back.
Patients are currently asked to arrive around 2 hours before the cataract operation is scheduled so that proper preparation can be done. Today, there is an increasing number of treatment protocols and innovations that enable patient waiting time and preparation to be reduced. In the “Standing Patient” circuit, the patient is not taken to the operating theatre on a trolley, but rather walks there unassisted. This enables them to retain their dignity and be actively involved in their treatment process. As for the “fast-track” circuit, this enables patient treatment stages to be improved and proceed more quickly.
Mydriasis (dilation of the pupil) is achieved either by the administration of eye drops 45 minutes to 1 hour before the actual cataract operation, or by means of an ophthalmic insert that shortens the time required to less than 30 minutes before surgery, or by means of an intra-ocular injection performed once inside the operating theatre.
Local anaesthesia is administered in the form of eye drops. The peri-ocular areas (around the eye) and the ocular surface (the eye itself) are disinfected using special antiseptic products.
Post-op care
Most patients report no eye pain after cataract surgery.
Eye drops for post-operative care are prescribed immediately after the operation. Patients must use them throughout the prescribed period, even if the eye looks completely normal. In addition, it is extremely important not to rub the eye on which cataract surgery has been performed, and you patient wear a protective eye patch at night while sleeping. This eye patch must be kept clean. Wash it with soap and water and leave to dry thoroughly between uses.
Ideally, eye makeup should not be applied for at least a week after the operation. You can resume normal visual activities the day after surgery, but swimming and strenuous physical activity is prohibited for the first two to three weeks following the operation. Patients should refrain from driving until they feel that their eyesight has returned to normal. However, travelling, including flying after cataract surgery, is allowed.
These recommendations will of course be adapted to particular medical prescription. The first point of contact, should you have any questions, is your ophthalmologist.
Vision normally improves after a few weeks. Regular eye tests are essential to make sure there are no complications. Glasses can be prescribed if your visual acuity remains impaired a few weeks after surgery. Tinted glasses can also help lessen any glare sensitivity problems you experience following the operation.
During the recovery period, your GP can prescribe sick leave if he/she deems it appropriate in view of your job and state of health.
Side effects
Blurred vision after cataract surgery is normal, but this should improve fairly quickly. Red eye after cataract surgery may also be possible, indicating slight haemorrhaging which will be reabsorbed and disappear after a few days.
Your eye may feel irritated, or feel as if it has sand or a foreign body in it. Similarly, you may feel some pain in your eye for 24 hours after cataract removal. You might also see “floaters” (medical name myodesopsia), experience increased light sensitivity and dry eyes, but these are temporary phenomena and will disappear.
Whatever the issue, your ophthalmologist will explain all the possible risks and complications to you in detail. Furthermore, should you experience any abnormal symptoms in the days following cataract removal (your eye is red, swollen or weeping pus), you should inform your GP immediately.
Several years after cataract surgery, the lens capsule (behind the intra-ocular implant) can sometimes become opaque. This is a secondary cataract that causes impaired visual acuity. Should this occur, it is most often treated with laser surgery.
Sources :
(1) Ameli, Le traitement de la cataracte [en ligne]. Disponible sur : www.ameli.fr/marne/assure/sante/themes/cataracte/traitement
(2) Ameli, Comprendre la cataracte [en ligne]. Disponible sur : www.ameli.fr/assure/sante/themes/cataracte/comprendre-cataracte.
(3) Haute Autorité de Santé, Fiche pertinence des soins indications et contre-indications de la chirurgie de la cataracte liée à l’âge [en ligne]. Disponible sur : www.has-sante.fr/jcms/c_2906983/fr/fiche-pertinence-des-soins-indications-et-contre-indications-de-la-chirurgie-de-la-cataracte-liee-a-l-age.
(4) Bérengère Deforge, Gilles Duluc, Julie Garnon, François Mourey, Mihail Ott, « Le parcours “patient debout” – L’expérience de l’hôpital Saint-Louis », Gestions hospitalières, Numéro 574, mars 2018.
(5) Haute Autorité de Santé, Conditions de réalisation de la chirurgie de la cataracte : environnement technique – Rapport d’évaluation technique, Juillet 2010 [en ligne]. Disponible sur : www.has-sante.fr/jcms/c_992026/fr/conditions-de-realisation-de-la-chirurgie-de-la-cataracte-environnement-technique-rapport-d-evaluation.
(6) ANAP, Premier Cercle SD – Bloc opératoire « Concilier qualité de prise en charge et efficience » – Mettre en œuvre la démarche « patient debout » au bloc opératoire [en ligne]. Disponible sur : http://bloc-operatoire.anap.fr/publication/2138.
(7) Jennifer Marie-Louise, Ramin Tadayoni, « Ophtalmologie : des progrès notables, des espoirs thérapeutiques, à quel coût ? », La Revue du Praticien Médecine Générale, Tome 67, n° 10, décembre 2017, pp. 1 097-1 106.
(8) Clémence Bonnet, Antoine Brezin, « Cataracte, quand opérer ? », La Revue du Praticien Médecine Générale, Tome 32, n° 1 000, mars 2018, pp. 326-327.


